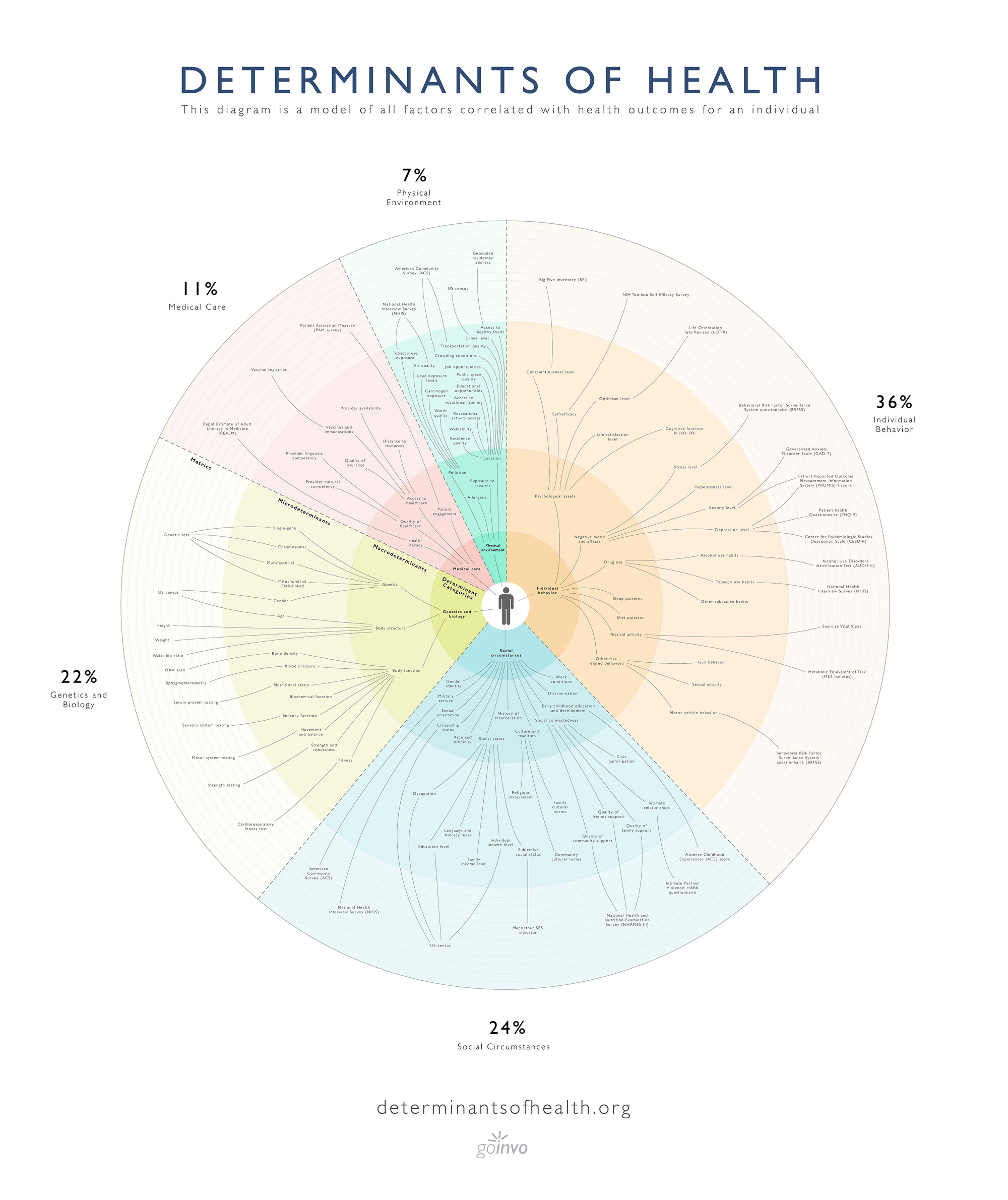
The social determinants of health (SDOH) are non-clinical factors that contribute to an individual’s health and well-being. Various institutions have different determinant definitions, but there is general consensus that most of an individual’s well-being is not attributed directly to the healthcare system.
There are recurring broad strokes amidst all of the literature here.
- Community health
- Behaviours & Social >> Clinical
- All domains of life lead to healthcare
- Maslov’s Hierarchy is King (if people have no jobs they’re going to be sick)
GoInvo
A healthcare UX firm based in the US, doing incredible research at the intersection of healthcare and design. Their open-source illustration is my go-to reference for the social determinants of health.
HealthyPeople.gov
An initiative by the US government “Healthy People 2020”.
The Social Determinants of Health topic area within Healthy People 2020 is designed to identify ways to create social and physical environments that promote good health for all.
Their five determinants include:
- Economic Stability
- Education
- Social and Community Context
- Health and Health Care
- Neighborhood and Built Environment
Literature Summaries on various determinant factors
Kaiser Family Foundation
KFF claims that it is a non-partisan source of facts and analysis, polling and journalism for policymakers, the media, the health care community, and the general public
The social determinants of healthcare in KFF literature
Social determinants of health are the conditions in which people are born, grow, live, work and age that shape health.

Some key takeways:
- Policies and practices in non-health sectors have impacts on health and health equity.
- “Health in All Policies” is an approach that incorporates health considerations into decision making across sectors and policy areas
- The Affordable Care Act established the National Prevention Council to develop the National Prevention Strategy
- There continues to be growing recognition of the relationship between neighborhoods and health, with zip code understood to be a stronger predictor of a person’s health than their genetic code.
The National Prevention Strategy
- The National Prevention Strategy lays out four strategic directions: healthy and safe community environments, clinical and community preventive services, empowered people (another way to say autonomous), and the elimination of health disparities.
Research should be in dynamic relation with local agents of change in the environment -> local-care-for-global-health
Other Related Meanderings: